Technological advances are rapidly transforming health care, driving the need for IT solutions that improve patient care while saving time and money.
One area where this progress stands out is medical billing.
Traditionally slow and error-prone, tasks like medical coding, claims submission, and payment reconciliation are being reshaped by new technology.
These innovations are helping healthcare providers, insurers, and patients see better results, according to industry experts.
The demand for smarter billing solutions continues to grow. From improving transparency and speeding up processes to reducing errors, healthcare professionals are moving away from outdated systems and turning to advanced tools that help them stay efficient, competitive, and compliant.
In this blog, we’ll explore 5 major technology trends that are redefining the future of medical billing services and how these trends are set to change the way billing works in the years ahead.
1. Artificial Intelligence (AI) and Machine Learning in Medical Billing
The Role of AI and ML in Healthcare
Artificial Intelligence (AI) and Machine Learning (ML) are becoming key tools in many areas of health care, and billing is no exception, especially for small practices.
By automating repetitive and time-consuming tasks, these technologies help make the billing process faster and more accurate while reducing human error.
AI-Driven Automation in Billing
One of the biggest advantages of AI in billing is automation. It allows providers to streamline processes like claim submission, error detection, and patient invoicing.
AI can review billing codes and patient data to ensure claims are properly coded before they’re sent to insurers, greatly reducing the risk of denials due to mistakes or missing information.
Machine learning takes things a step further by learning from past claim errors and continuously improving over time.
These models can spot patterns and predict issues before they happen, alerting teams to problems like mismatched patient details, incomplete documentation, or incorrect codes.
By analyzing historical data, ML can also identify which claims are likely to be rejected or delayed, giving billing teams time to address potential issues in advance.
Together, AI and ML are helping practices create faster, more accurate billing systems that require less manual work and lead to better results.
3 Benefits of AI and ML in Billing
- Reduced error rate: This kind of AI simply increases the accuracy of some of the most complicated tasks by analyzing data input with specialized algorithms and spotting any inconsistencies in real time.
- Faster processing: Thanks to AI, some path-breaking billing tools are able to take up activities such as data entry and claim submission in their stride, thereby expediting the billing cycle.
- Improved cash flow: With fewer claim denials and faster payments, cash flow for healthcare providers becomes easier.
2. Blockchain Technology: Ensure Security and Transparency
How Blockchain Works in Healthcare
While often linked to cryptocurrencies, blockchain technology is increasingly being used in health care for secure and reliable record-keeping.
As a decentralized system for managing and storing billing data, blockchain offers a fresh approach to how billing processes are handled.
Blockchain for Secure Billing Systems
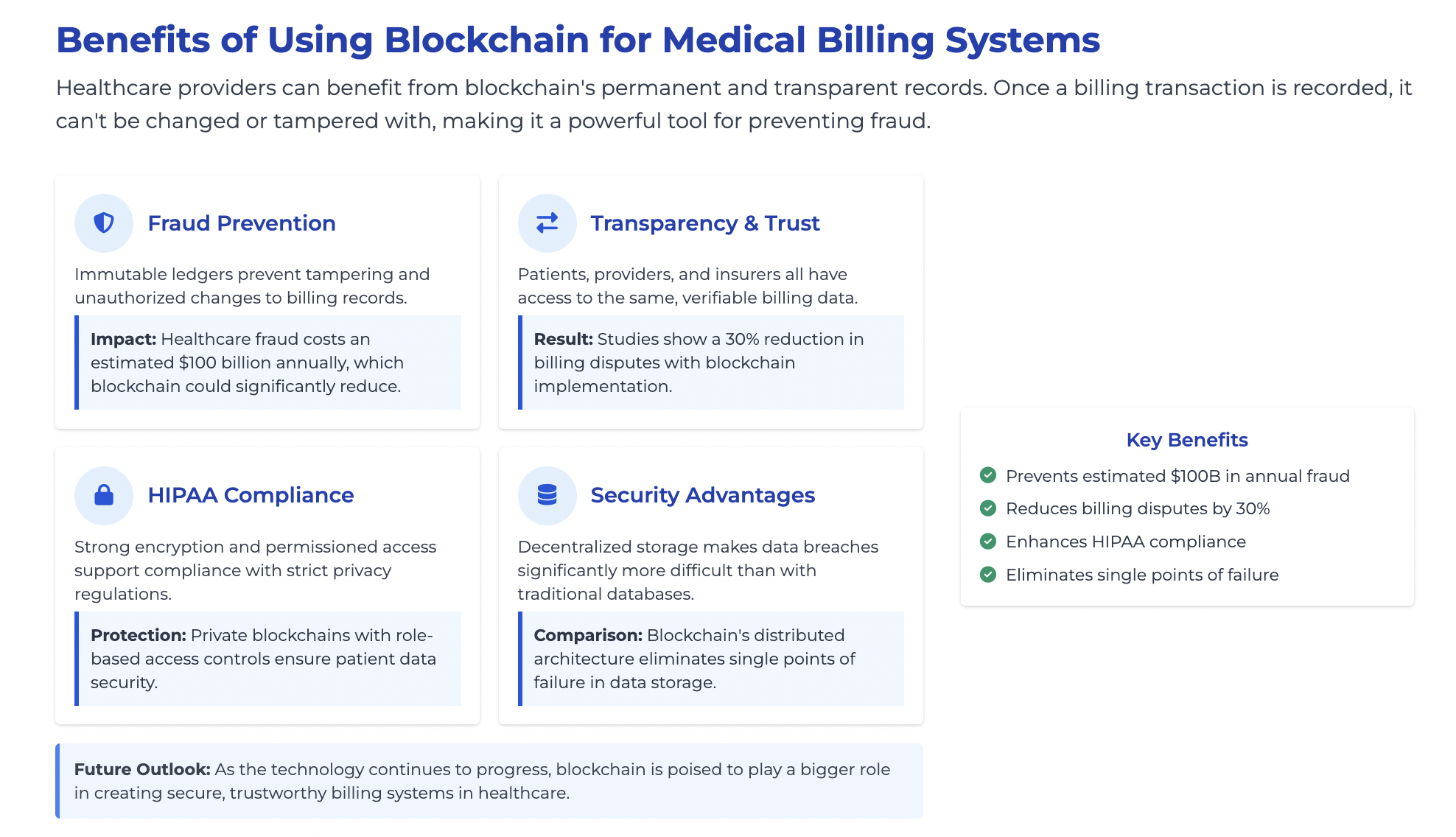
Healthcare providers can benefit from blockchain’s permanent and transparent records.
Once a billing transaction is recorded, it can’t be changed or tampered with, making it a powerful tool for preventing fraud.
Patients, providers, and insurers all have access to the same, verifiable version of billing data, helping to build trust and reduce disputes.
Beyond transparency, blockchain also enhances data security. Billing data often contains sensitive patient information, so protecting that information is important.
Through strong encryption and decentralized storage, blockchain supports compliance with strict privacy regulations like HIPAA, offering a higher level of security than traditional databases.
As the technology continues to progress, blockchain is poised to play a bigger role in creating secure, trustworthy billing systems in health care.
Advantages of Blockchain in Medical Billing
- Increased transparency: Real-time visibility into transactions can help resolve billing disputes quickly.
- Fraud prevention: Blockchain’s immutability ensures that billing data cannot be manipulated, minimizing fraud risks.
- Faster reimbursements: Blockchain can streamline the payment process by automating transactions between parties.
3. Cloud-Based Medical Billing Solutions
The Shift to Cloud Computing in Healthcare
Cloud technology is making a strong impact in health care, offering a modern way to manage and store data.
Billing operations, in particular, are benefiting from the flexibility, scalability, and remote access that cloud systems provide.
Benefits of Cloud-Based Billing Solutions
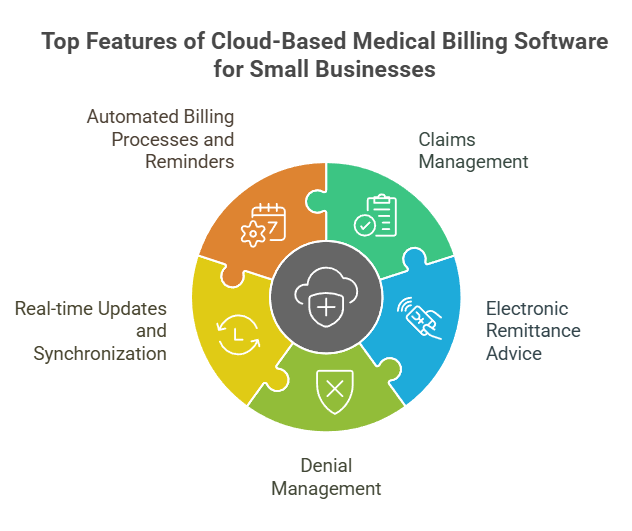
One of the main strengths of cloud-based billing is its ability to scale with ease.
Whether it’s a solo practice or a large hospital network, cloud platforms can adapt without the need for major infrastructure upgrades.
These systems also enable secure, real-time access to billing data from any location: an important feature for multi-site providers and teams working remotely.
Another advantage is automatic updates. Cloud solutions are often kept current with the latest billing codes and compliance requirements, helping reduce the risk of costly errors.
This ensures that healthcare providers stay up to date with changes in CPT (Current Procedural Terminology) and ICD (International Classification of Diseases) codes without manual intervention.
With its combination of convenience, reliability, and efficiency, cloud computing is proving to be a valuable asset in modernizing the billing process.
Key Benefits of Cloud-Based Billing
- Remote access: Billing can be modified and reviewed from anywhere, which will mean it is much easier to collaborate with staff and have current access to all information.
- Cost-effective: Cloud systems reduce the need for expensive on-premise infrastructure, with subscription-based pricing that scales with usage.
- Automatic compliance updates: Cloud solutions ensure that medical billing practices remain in compliance with constantly changing laws and coding standards.
4. Robotic Process Automation (RPA) to Streamline Billing Tasks
What is Robotic Process Automation (RPA)?
Robotic Process Automation (RPA) is a technology that uses software “bots” to handle repetitive, rules-based tasks typically performed by humans.
In healthcare, this includes routine administrative work like claims submission, follow-up communication, and payment posting.
These bots can perform actions such as filling out forms, making calculations, or tracking the status of claims, saving time and reducing human error.
RPA’s Impact on the Medical Billing Process
RPA is especially effective in areas that involve repetitive, manual steps, particularly when tasks follow a consistent set of rules.
For example, once a claim is submitted, bots can monitor its progress, flag items that are pending or rejected, and even identify preauthorized claims.
They can also send automated follow-up messages to help keep the process moving without delays.
By handling these routine activities, bots free up billing staff to focus on more complex issues, like managing denied claims or working through negotiations with payers.
The result is a more efficient workflow, fewer delays, and better use of staff time.
How RPA Improves Billing Efficiency
- Reduced manual effort: RPA bots can handle repetitive tasks, allowing staff to focus on more strategic activities.
- Improved accuracy: Bots execute tasks with high accuracy, reducing the likelihood of human error in billing processes.
- Faster claim processing: RPA accelerates the claims process by automating data entry and follow-up tasks, leading to faster reimbursements.
5. Telemedicine and Remote Patient Monitoring in Billing
Telemedicine’s Impact on Medical Billing
Telemedicine has seen rapid growth, especially since the COVID-19 pandemic pushed virtual care into the mainstream.
As more providers offer remote visits, billing systems must adapt to support telehealth services effectively.
Telemedicine Billing Codes and Reimbursement
To receive proper reimbursement for virtual care, providers must use specific billing codes and update their systems to include telemedicine-related contracts.
Many are working to integrate these requirements into their existing Electronic Health Records (EHR) and Practice Management Systems (PMS), so that virtual visits are documented and billed just like in-person appointments.
Remote Patient Monitoring (RPM) Billing
Similar to telemedicine billing, Remote Patient Monitoring (RPM) has also gained momentum. It involves using connected devices to track patient health (like vital signs or chronic conditions) from home.
Billing for RPM requires the use of multiple codes and a separate reimbursement process.
To handle this effectively, providers need a clear workflow that incorporates RPM data into their billing systems, ensuring services are properly recorded and reimbursed.
Benefits of Telemedicine and RPM in Medical Billing
- New revenue streams: Telemedicine and RPM open up new revenue opportunities for healthcare providers by offering remote care services.
- Faster reimbursement: Telemedicine and RPM can speed up billing processes through automation and accurate coding.
- Patient convenience: These technologies allow patients to access care remotely, reducing the need for in-person visits.
Conclusion: Embrace the Future of Medical Billing
As health care continues to evolve, billing and reimbursement systems must keep pace.
Advances in AI, blockchain, cloud computing, RPA, and telemedicine are reshaping how billing is handled, bringing greater efficiency, security, and transparency to the process.
At Physicians Revenue Group, Inc., we’re proud to be at the forefront of this transformation. Whether supporting small practices or large healthcare systems, we leverage cutting-edge technology to streamline billing, speed up turnaround times, and improve financial outcomes.
By prioritizing accuracy and compliance, we help our clients achieve faster recoveries and long-term success.
Innovation is all about supporting better care and a stronger healthcare system overall.